Updated on February 15, 2023
Lung cancer is the leading cause of cancer-related death in both men and women in the United States. In 2023, an estimated 238,340 people will be diagnosed with the disease and more than 127,000 will die, according to the American Cancer Society.
Although the numbers may sound staggering, it's worth noting that up to 90 percent of lung cancer cases are preventable. That’s because the primary cause of lung cancer is smoking cigarettes. According to the Centers for Disease Control and Prevention, the habit is associated with up to 90 percent of lung cancer diagnoses.
“If you smoke a pack a day for 30 or 40 years, you're 20 times more likely than somebody who's never smoked to develop lung cancer,” says Erev Tubb, MD, a medical oncologist and hematology specialist at Inspira Medical Center Mullica Hill in New Jersey.
The good news? Quitting smoking can reduce your risk of developing lung cancer. And it’s never too late to kick the habit.
“For years, the mortality rates for lung cancer were rising dramatically, but smoking cessation is actually the reason why they’re starting to go down,” explains Dr. Tubb.
But smoking isn’t the only risk factor for lung cancer. Exposure to certain environmental hazards—like radon, asbestos, and air pollution, not to mention secondhand smoke—can also play a role, as can other factors including a family history of the disease.
Know the signs of lung cancer
If you’re at increased risk of developing lung cancer, it’s important to become familiar with certain signs and symptoms of the disease, such as:
- Persistent or worsening cough
- Cough that produces blood or rust-colored mucus
- Chest pain that worsens when breathing deeply, coughing, or laughing
- Shortness of breath or new onset of wheezing
- Hoarseness
- Fatigue or weakness
- Persistent lung infections like bronchitis or pneumonia
There are a number of additional symptoms that may not seem related to lung cancer that may also be indicators. These include:
- Decreased appetite
- Weight loss
- Bone pain
- Blood clots
Making a diagnosis can be difficult
The trick is, these general warning signs—and even the respiratory symptoms—are not necessarily specific to lung cancer.
“The majority of people with lung cancer have a cough. Some are short of breath and some may have chest discomfort,” says Tubb. “But these are all things that can be found in conditions other than lung cancer.” For example, many of these symptoms could be related to asthma, pneumonia or even a cold.
What’s more, by the time many of these symptoms arise in a lung cancer patient, it’s often an advanced form of cancer.
“Our bodies have great respiratory capacity to the point where it really has to be decreased by a significant amount before you start feeling short of breath,” says Tubb.
And therein lies the problem with relying exclusively on symptoms to make a diagnosis.
“By the time you’ve lost 40 percent of your lung capacity,” he says, “the disease has already had a chance to advance significantly. You may not feel symptoms like shortness of breath until you’ve lost that capacity.”
On top of that, the lungs have very few nerve endings, which means if a cancerous tumor grows in the lungs, it may go undetected because it typically won’t cause any noticeable pain or discomfort.
Aside from quitting smoking and avoiding the type of environmental exposures that can increase your risk, the best thing you can do for your health is to identify lung cancer before you even start to experience symptoms. The earlier the cancer is detected, the better chance you have for successful treatment.
The value of screening for lung cancer
The good news is that screening for lung cancer may help with making a diagnosis. But there are a few caveats worth keeping in mind.
One large clinical trial known as the National Lung Screening Trial (NLST) was conducted to investigate the best screening method to help reduce lung cancer-related deaths.
“Up to this point, there was really no good way to screen for lung cancer,” says Tubb. “Physicians would do chest X-rays, but there was no clear evidence that chest X-rays detected anything except for later-stage cancers.”
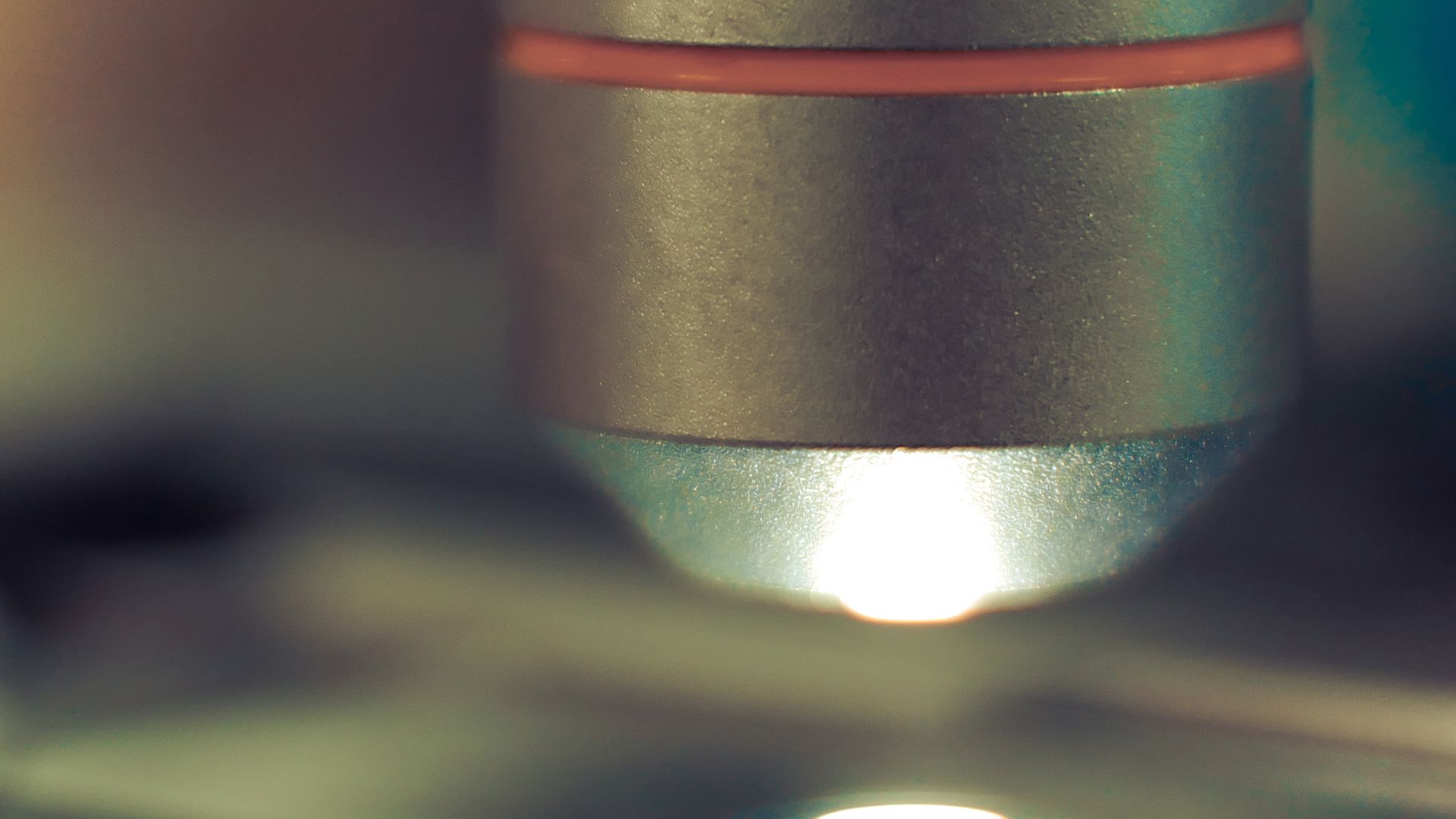
The NLST compared the effects of low-dose computed tomography (CT) scans with those of X-rays. The initial results, released in November 2010, found that the CT scans provided more detailed imaging and were better at detecting small abnormalities in the lungs than X-rays. The study authors concluded that the scans could help lower the risk of dying from lung cancer.
These CT scans aren’t perfect, however. While they can detect something very small, there’s a chance that whatever is detected may not even be related to lung cancer. This can eventually lead to additional, potentially unnecessary testing.
Most lung masses that are detected in CT scans—particularly those considered small, or less than 9 millimeters in diameter—are not actually cancer. In fact, fewer than 5 percent of small nodules turn out to be cancer. These small masses are often simply a sign of a previous infection, scar tissue or the like. When they are picked up by a CT scan, this is known as a false positive result. The only way of knowing for sure is to undergo a follow-up scan or additional testing.
“Say the CT scan finds something that’s 5 millimeters, which is very small,” Tubb says. “You can’t actually biopsy a 5-millimeter lesion. You have to wait a little bit to see if it goes from 5 to 10 millimeters from one scan to the next.”
CT scans are thus not often a “one and done,” explains Tubb.
“If a spot is seen at 5 millimeters, it could be benign or it could be malignant,” he says. “There’s no way to determine that on the spot. So, what’s done is usually a follow-up scan at a shorter interval than the usual screening test to see if it’s grown or not.”
It’s important, therefore, to coordinate your care with a surgeon in order to determine the optimal timeframe for removing a suspicious nodule as opposed to proceeding with a biopsy, says Tubb.
Who should get screened?
Because lung cancer screening is not necessarily beneficial for everyone, whether or not you should undergo screening really depends on your individual health history.
“The number one thing you can do is talk to your doctor about how they can help you,” says Tubb. Your doctor will then work with you to discuss potential next steps for evaluation and screening that are suited to your circumstances.
The best candidates for lung cancer screening are those who are at high risk for developing the disease. According to guidelines released by the U.S. Preventive Services Task Force (USPSTF) in March 2021, this includes people between the ages of 50 and 80 who also:
- Smoke cigarettes currently or have only quit within the past 15 years
- Have a history of smoking the equivalent of one pack of cigarettes per day for 20 years
According to the USPSTF, screening should take place every year. It should stop once a person has not smoked for 15 years or develops a health problem that limits their life expectancy or the ability to have lung surgery to treat the problem. Patients should be informed of the benefits, limitations, and potential risks of low-dose CT scans for lung cancer screening and have access to a facility that provides screening and treatment.
Regular CT screening for older heavy smokers has proven effective in studies. In the NLST trial, having annual CT scans was linked to a 20 percent lower risk of dying of lung cancer, compared to getting annual chest X-rays.
The results were even better in a study published in the New England Journal of Medicine in 2020. European researchers found that over a 10-year period, having heavy smokers aged 50 to 74 get regular CT scans cut deaths by 33 percent for women and 24 percent for men.
In the end, if you are ultimately diagnosed with lung cancer, the earlier you catch it, the more curable it may be.
“Even in advanced stages,” says Tubb, “there is hope for longer-term survival based on good responses to newer therapies for lung cancer.”